For the human body to function smoothly, every organ and joint must work in harmony. When even a single part is injured or affected, it can disrupt everyday activities and reduce overall quality of life. One of the most commonly affected areas is the shoulder joint. Known for its wide range of motion, the shoulder is also one of the most complex joints in the body. While this mobility is essential for performing daily tasks, it also makes the shoulder more vulnerable to injuries and conditions.
When shoulder pain, stiffness, or injury begins to interfere with routine life, doctors often recommend shoulder arthroscopy—a minimally invasive procedure used to both diagnose and treat shoulder problems.
This article will help you understand shoulder arthroscopy in detail—what it is, when it’s recommended, its benefits, and the recovery process.
What is Shoulder Arthroscopy?
Shoulder arthroscopy is a surgical technique that uses small incisions and a tiny camera (arthroscope) to examine and treat shoulder issues. The arthroscope allows the surgeon to see inside the joint with precision, ensuring accurate diagnosis and treatment with minimal damage to surrounding tissues.
Unlike open surgery, which requires large incisions, shoulder arthroscopy is minimally invasive, reducing risks, pain, and recovery time. Patients often return home the same day and resume light activities within a short period, though full recovery depends on the condition being treated.
When is Shoulder Arthroscopy Suggested?
Doctors usually recommend shoulder arthroscopy when non-surgical treatments such as physiotherapy, medications, or steroid injections fail to provide relief. Common conditions where arthroscopy is suggested include:
- Shoulder impingement syndrome – when tendons rub against bones, causing pain.
- Recurrent dislocations or instability – when the shoulder frequently “slips out” of place.
- Rotator cuff tears – partial or complete tears of shoulder tendons.
- Frozen shoulder (adhesive capsulitis) – stiffness and reduced movement in the joint.
- Arthritis or osteoarthritis – degenerative changes in the shoulder joint.
- Bursitis – inflammation of the fluid-filled sacs cushioning the joint.
Conditions and Injuries Treated with Shoulder Arthroscopy
Shoulder arthroscopy can address a wide range of injuries and conditions, including:
- Bicep tendon injuries – inflammation or tears in the tendon connecting the bicep to the shoulder.
- Bone spurs – excess bone growths causing friction and pain.
- Labral tears – injuries to the cartilage rim of the shoulder socket.
- Rotator cuff injuries – ranging from small frays to complete tendon tears.
- Shoulder impingement – pinching of tendons or tissues.
- Osteoarthritis – wear and tear of cartilage leading to pain and stiffness.
- Shoulder instability or frequent dislocations – common in athletes or after accidents.
Preparing for Shoulder Arthroscopy
Before undergoing surgery, the doctor will review your medical history and run diagnostic tests to ensure you’re fit for the procedure. Preparation may include:
- Blood tests – to check overall health and detect hidden conditions.
- ECG (Electrocardiogram) – to assess heart health, especially in older patients.
- X-rays or MRI scans – to evaluate the extent of damage inside the shoulder.
Doctors may also provide pre-operative instructions, such as fasting before surgery, avoiding certain medications, or arranging post-surgery assistance at home.
Is Shoulder Arthroscopy Painful?
While all surgeries involve some discomfort, shoulder arthroscopy is designed to minimize pain. To ensure comfort, surgeons use:
- Nerve blocks – injections around the neck or shoulder to numb the area and reduce pain even after surgery.
- General anesthesia – in some cases, patients are put to sleep during the procedure.
Post-surgery, pain medications and ice packs are recommended to control swelling and discomfort, making the recovery process smoother.
Benefits of Shoulder Arthroscopy
Compared to traditional open surgery, shoulder arthroscopy offers numerous advantages:
- Minimally invasive – small incisions mean less tissue damage.
- Faster recovery – patients often return to normal activities within weeks.
- Minimal scarring – tiny cuts leave little to no visible marks.
- Lower risk of infection – smaller wounds reduce complications.
- Less stiffness – improved mobility post-surgery.
- Shorter hospital stay – many patients return home the same day.
Post-Surgery Care and Recovery
While shoulder arthroscopy is a short procedure (usually under an hour), proper recovery steps are crucial for long-term success.
Wound Care
- Keep the wound dry for at least 48 hours.
- Avoid removing surgical strips or visible sutures prematurely.
- Call your doctor if you notice redness, swelling, or excessive pain.
- Ice the area for 20 minutes, 3–4 times a day, to reduce swelling.
Mobility and Exercise
- Begin physiotherapy exercises as instructed by your doctor.
- Passive range-of-motion exercises help restore flexibility.
- Light activities can be resumed within days, but heavy lifting should be avoided until cleared by the surgeon.
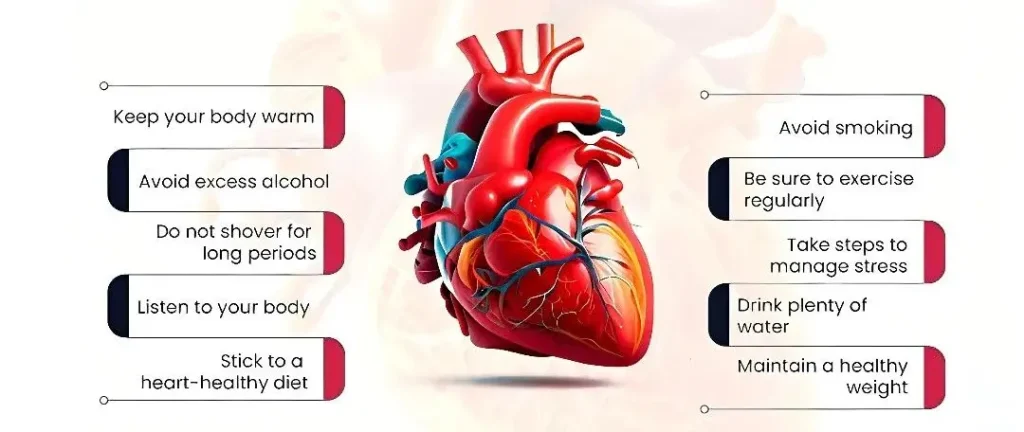
Dietary and Lifestyle Precautions
- Start with liquids immediately after surgery; progress to solids gradually.
- Eat light meals to avoid nausea caused by anesthesia.
- Adequate hydration helps speed up healing.
Sleep and Comfort
- Sleep with your shoulder elevated using pillows or in a recliner.
- Wearing a sling for 2–3 weeks is common to protect the joint.
- Sleep disturbances may occur for a few weeks but improve with healing.
Conclusion
Shoulder arthroscopy is a safe, effective, and minimally invasive solution for treating a wide range of shoulder problems. With proper preparation, skilled surgical care, and consistent post-operative rehabilitation, patients can experience significant pain relief, improved mobility, and a return to normal daily activities within weeks.
At Oxford Hospital, we specialize in advanced orthopedic procedures like shoulder arthroscopy. Our team of experienced doctors ensures precise diagnosis, expert surgical care, and personalized rehabilitation plans to help patients regain strength and mobility with confidence.