Myth 1: Can a stent move or slip from the position where it was implanted?
Fact: No, the stent is securely implanted in the artery using a balloon at high pressure. Over the next few weeks, the stent becomes embedded within the artery lining, essentially becoming part of the artery, so there is no risk of it moving.
Myth 2: Can a stent rust inside the body since it is made of steel?
Fact: No, stents are made from a special type of medical-grade, rust-proof steel. Modern stents are typically crafted from materials like cobalt chromium or platinum, which do not rust inside the body.
Myth 3: Can a stent be deformed by external pressure on the chest, or will it pinch the heart or nearby organs?
Fact: No, the heart is located within the chest cavity, and no external pressure can affect the stent positioned inside the artery. Once placed, the stent is embedded within the artery lining and cannot pinch or impact any other part of the body.
Myth 4: Can I have an X-ray, CT scan, or MRI after stenting?
Fact: Yes, X-rays and CT scans can be done at any time after stenting, and MRIs are safe after one month.
Myth 5: Will a metal stent trigger alarms during security checks, like those at airports?
Fact: No, it will not.
Myth 6: Can a stent become blocked again after angioplasty, and how can I prevent it?
Fact: Yes, there is a slight chance of re-blockage. The risk of clot formation is about 0.5%, and the risk of restenosis (re-narrowing) is 5% to 15% for drug-eluting stents (DES) and bare-metal stents (BMS), respectively.
Myth 7: Can I return to a healthy, normal life after angioplasty?
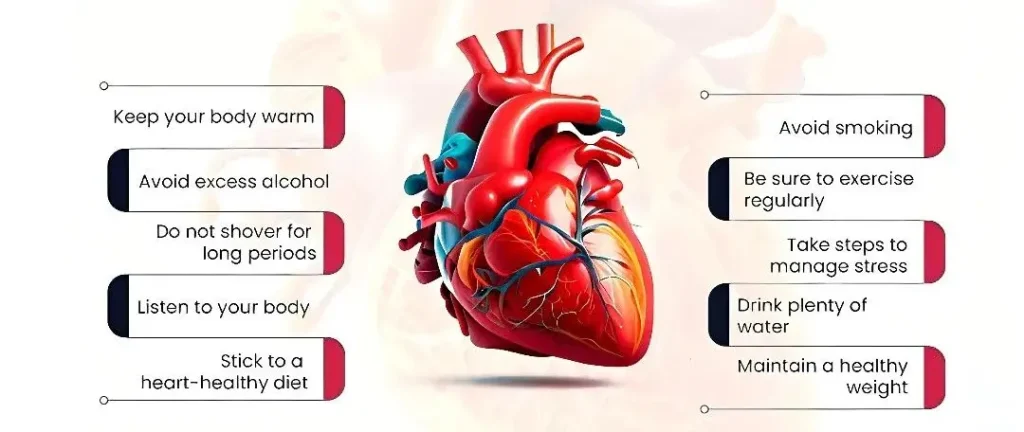
Fact: Absolutely. Most people can resume their regular lifestyle within a few days if they haven’t experienced a heart attack and have a heart ejection fraction above 50%. Adopting a heart-healthy diet, regular exercise, and other lifestyle changes can accelerate recovery and reduce the chances of restenosis.
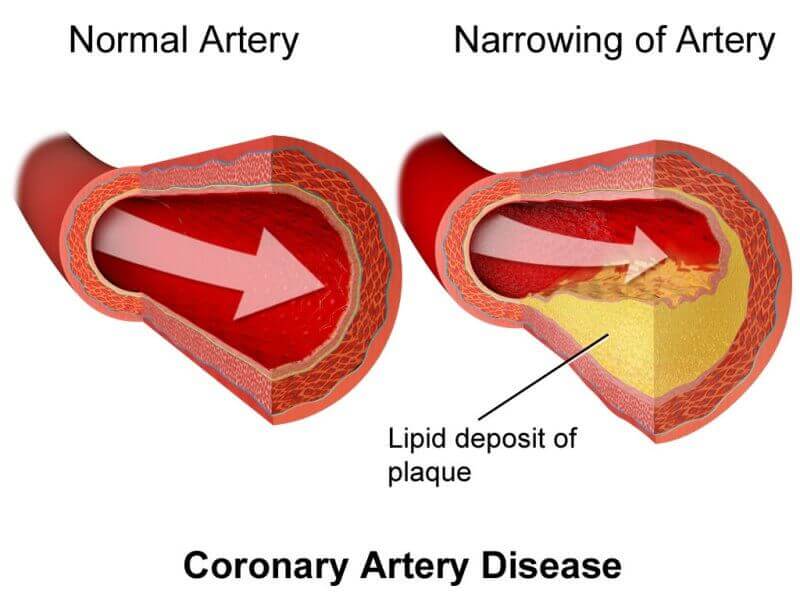
Myth 8: Is there a chance of developing coronary artery disease (CAD) again?
Fact: Angioplasty clears dangerous blockages, but other parts of the artery or other arteries may still accumulate deposits over time. While no one can guarantee CAD won’t recur, controlling risk factors like diet, exercise, blood pressure, and diabetes greatly reduces the risk.
Myth 9: Does taking aspirin daily help prevent heart attacks?
Fact: Yes, daily aspirin can reduce the risk of heart attacks and strokes by thinning the blood. However, it should be taken under a doctor’s guidance for the correct dose and duration.
Myth 10: Is the prolonged exposure to X-rays during angioplasty harmful?
Fact: No, the angiography and angioplasty procedures are performed using a specialized device called a Cardiac Cath Lab, which emits only the minimal necessary dose of radiation. The X-ray dosage is carefully monitored, ensuring it is safe for the patient.
Myth 11: At what level of artery blockage should angioplasty be performed, and can it treat a 100% blocked artery?
Fact: Angioplasty is generally recommended for blockages over 70%. Although 100% blocked arteries can also be treated with angioplasty, the procedure is more complex in such cases. Your doctor will assess and decide on the best approach for each blockage.
Myth 12: If I feel fine, should I still be concerned about high blood pressure?
Fact: Yes, high blood pressure is often called a “silent killer” because many people are unaware they have it until a doctor detects it, even though it can silently damage organs. Uncontrolled blood pressure can increase the risk of restenosis after angioplasty.
Myth 13: Can I continue smoking after angioplasty?
Fact: No. Smoking significantly raises the risk of blood vessel constriction, which is especially dangerous for already narrowed arteries. Quitting smoking is essential to protect your health.
Myth 14: Is it normal to feel anxiety after angioplasty?
Fact: Yes, post-procedure anxiety is common, with concerns ranging from fleeting chest pains to general worry about health. It’s normal, but try to stay positive and avoid overthinking. Consult your doctor if anxiety persists.
Myth 15: When can I return to work after angioplasty?
Fact: Most patients can resume work within a week. The type of work suitable depends on the extent of recovery and the nature of your job. Less physically demanding tasks are recommended initially, but your doctor will provide personalized guidance.
Myth 16: How should I handle depression that I’m experiencing?
Fact: If you’re noticing signs of depression, such as:
– Sleep disturbances
– Appetite changes
– Fatigue
– Emotional stress
– Loss of focus or alertness
– Apathy
– Low self-esteem
– Feelings of despair
– Disorganization
It’s important to consult with your doctor, who may prescribe medication or recommend other appropriate treatments.
Myth 17: How much alcohol can I safely consume?
Fact: If you don’t drink, it’s best not to start. Moderate alcohol consumption is generally fine, but excessive drinking can raise blood pressure and negatively affect your health.
Myth 18: When can I resume sexual activity after angioplasty?
Fact: If you’re able to climb two sets of stairs without experiencing shortness of breath, you can generally resume sexual activity.
Myth 19: What kind of diet should I follow after angioplasty?
Fact:
1. Avoid fried, fatty foods, especially those containing trans fats.
2. Increase your intake of vegetables and fruits.
3. Opt for whole grains and high-fiber foods.
Myth 20: What is a healthy caloric intake for me?
Fact: Your daily calorie intake should be between 1200 and 2000 calories, depending on your ideal body weight and BMI, as advised by a dietitian. Focus on plenty of vegetables and fruits, up to 50 grams of nuts, and choose polyunsaturated or monounsaturated fats found in refined oils. Avoid saturated fats (found in whole milk, butter, ghee, and sweets) and trans fats (found in fast foods and bakery products). Limit salt intake, especially in processed foods, as it often contains double the amount of sodium.
Myth 21: What kind of exercise is safe after angioplasty?
Fact: Avoid isometric exercises like weight lifting, dumbbells, or bench presses. Isotonic exercises, such as walking, swimming, and cycling, are ideal for heart patients. Exercise intensity and duration should be based on individual capacity, with a focus on symptom-limited activity in the first few months.
Yoga is also a great option for heart health, offering several benefits:
– Gentle yoga stretches muscles, improving insulin sensitivity, which is crucial for managing blood sugar.
– Deep breathing techniques can help lower blood pressure.
– Mind-calming meditation quiets the nervous system, reducing stress.
All of these practices can help prevent heart disease and support those with cardiovascular issues.